This is a broad topic and does not form part of the routine training of medical staff, so it is usually best dealt with by a dental general practitioner. However, current NHS dentistry provision is increasingly patchy, so such problems are presenting to medical primary care and emergency departments more frequently. In this record, you will find basic information on the presentation and initial management of dental and periodontal disease as well as notes on systemic conditions that affect the teeth and gums.
You may also want to refer to the separate articles Problems in the Mouth and Oral Ulceration.

- Local causes - this usually arises as a result of irritation of the nerve supplying the affected tooth. This can be due to a number of local problems, including inflammation of the pulp (pulpitis), infection and, most commonly, decay. Gum disease, grinding teeth (bruxism), tooth trauma and an abnormal bite are also causes. In babies and young children, consider the growth of unerupted teeth.
- Systemic causes - systemic problems should also be borne in mind. Think of temporomandibular joint, sinus or ear infections and tension in the facial muscles which can cause discomfort that resembles a toothache (these are often accompanied by a headache). Angina should also be considered in your list of differentials.
- Management - once you are sure that this is a local problem, it is appropriate to refer to a dental practitioner. Whilst waiting to be seen, advise patients to take regular oral analgesia (non-steroidal anti-inflammatory drugs (NSAIDs) are a good starting point) and some patients find that application of a cool compress on the cheek overlying the affected tooth helps.

- Nature of the problem - dentine is protected by a hard layer of enamel but if this is broken then caries follows. This can result from trauma or inadequacy of the enamel; the most common cause of breakdown of enamel is by lactic acid that is formed by bacteria when sugars are left in contact with the teeth. Risk factors are therefore a diet high in sugars and poor dental hygiene. Dental caries (or decay) is a common problem in all industrialised and in many developing countries. In the UK, a survey found that 40% of 5 year-olds had experienced some dental caries,[1] with Scottish preschool children experiencing some of the highest rates of dental caries in Europe.[2]
- Treatment - destroyed structures of the tooth do not regenerate so treatment is aimed at preventing further decay. Decayed material is removed by drilling and a substance is used to fill the tooth. Many different materials are now available, including silver amalgam, gold and high-strength composite resin. Crowns are used if decay is extensive and there is limited tooth structure which may cause weakened teeth. The decayed or weakened area is removed and repaired and a covering jacket or crown is fitted over the remainder of the tooth. Crowns are often made of gold, porcelain or porcelain fused to metal. If the nerve root dies a root canal filling may be required.
- Prevention - attention to diet and regular tooth
brushing are the main preventative strategies. There is a wealth of
material concerning dietary factors, particularly in young children. In
summary:[2]
- Human breast milk and unmodified cow's milk are not cariogenic, unlike infant formula milk (theoretically, soya infant formula milk is the worst offender).
- Drinks containing free sugars (including natural fruit juices) are cariogenic and shouldn't be given in a bottle.
- Foods and confectionary containing free sugars should be minimised and restricted to meal times.
- Cheese may actively protect against caries and is a good high-energy source for toddlers.
- Sugar substitutes are better for teeth than free sugars although beware of salt content and additives used to make the food as appealing.
Fluoridation
There has been a lot of research into the fluoridation of products and
its protective effects against dental caries. For example, fluoridation
of toothpastes, mouth rinses, gels and tooth varnishes has been common
practice for several decades, resulting in beneficial effects where
these products have been used appropriately.[1] Previous research over some 50 years has shown that adding fluoride to water supplies can reduce decay by 40-60%.[3]
1 part per million is required and, in those areas where there is
fluoridation of water, children aged under 7 should use lower fluoride
toothpaste. The fluoridation of water, however, remains politically
controversial and there are organised campaign groups both 'for'[4] and 'against'.[5]
No more than 10% of the country receive fluoride in their water. The
favoured areas are mostly in the north-east of England and the Midlands.
In 2004 health ministers were still insistent that fluoridisation of
water supplies is a matter for local decision and this remains the case
to date. It is the responsibility of strategic health authorities to
bring pressure upon local water boards. Fluoridation of milk and salt
has also been examined as a possible approach although the effectiveness
of such measures is yet to be proven. It is worth noting that fluoride
supplements taken by a pregnant woman have no beneficial effects on the
child's teeth.[2]
Numerous other areas of research are being explored for the prevention
of dental caries, including the development of various fillings,
antibacterial agents and fissure sealants.[6]
- Nature of the problem - this is a collection of pus in the tooth or within the surrounding structures. It most commonly originates in the centre (pulp) of the tooth - a periapical or dentoalveolar abscess. A periodontal abscess originates in the tissue surrounding the tooth. Their pathophysiology and management are different but, in the context of primary care, they can be treated as the same entity.
- Presentation - a dental abscess presents with
worsening pain (hours to days) which may radiate to the ipsilateral ear,
jaw and neck. There may be a bad taste in the mouth, fever ± malaise
and trismus (inability to open the mouth). It is more likely to occur
where there are risk factors for dental caries (see 'Dental caries'
above) and a history of previous dental procedures.
Other risk factors include diabetes, immunocompromise, smoking and
drug-induced gum disorders. Look for facial swelling, regional
lymphadenopathy, altered tooth appearance and gum swelling. Alternative
diagnoses to consider include:
- Infections such as mumps sinusitis acute otitis media and facial cellulitis.
- Salivary gland disorders such as a stone, infection (parotitis) or dehydration/dry mouth.
- Intraoral or salivary gland neoplasm.
- Management in primary care - the patient needs to
be seen by a dental practitioner. In the interim, pain can be managed
with regular analgesics such as NSAIDs (advise ibuprofen or naproxen in patients at risk of cardiovascular adverse events[7]).
Advise the patient to consume cool, soft food and to avoid very hot or
cold foods and drinks. Patients should avoid flossing the affected
tooth. Consider antibiotics only in the absence of immediate attention
by a dental practitioner and if:
- The infection appears to be severe (fever, lymphadenopathy, cellulitis, diffuse swelling).
- Patients are at risk of developing complications (eg people who are immunocompromised or diabetic or have valvular heart disease).
Wisdom teeth and their problems
Impacted wisdom teeth should not be removed unless they have
associated significant dental or other oral disease. Conditions
warranting removal of impacted wisdom teeth include:[8]
- Unrestorable caries.
- Non-treatable pulpal and/or periapical pathology.
- Cellulitis, abscess and osteomyelitis.
- Internal/external resorption of the tooth or adjacent teeth.
- Fracture of the tooth.
- Disease of the tooth follicle (ectomesenchymal tissue surrounding the developing tooth germ) including cyst/tumour.
- Tooth/teeth impeding surgery or reconstructive jaw surgery.
- When a tooth is involved in, or within the field of, tumour resection.
A post-extraction bleeding tooth socket should be treated by using a
wad of wet gauze placed over the socket and the patient should be
advised to bite down and arrest the haemorrhage through pressure; any
medications that promote bleeding should be considered for temporary
discontinuation and the patient should seek dental advice if the
symptoms do not settle, as suturing may be necessary.
Trauma
- Tooth loss: permanent dentition - traumatic tooth loss should be managed in adults and children with permanent teeth, initially, by trying to replace the tooth in the socket. If this is not possible, store the tooth in milk or the patient's own saliva. Attendance at a dental clinic as soon as possible (within 24 hours) gives a chance of replacing the avulsed tooth successfully.
- Tooth loss: primary dentition - in children with 'milk teeth', replacement of the tooth is not advised due to the danger of damaging the underlying permanent tooth. Store the avulsed tooth in saliva or milk and get the patient to attend a dental practitioner as soon as possible. A five-day course of antibiotics is recommended in this situation.[9]
- Dental concussion - the tooth is said to be concussed when there is damage to the supporting tissues without abnormal loosening or displacement of the tooth. Pulp necrosis may ensue (seen as the tooth going dark). This should be managed by a dental practitioner. Where the tooth is left as it is (common where a primary tooth is involved), the key thing is to advise parents to look out for swelling of the gum around the tooth; this may be an early manifestation of inflammation ± infection.
- Problems with fillings and crowns - these can be affected by external trauma (eg a fall). This is likely to be associated with more extensive injury - or by more minor trauma, eg biting on a hard fragment of food. It is best to get the tooth checked out by a dental practitioner, as loosening or chipping of the filling results in pain in the short-term and risk of further dental caries later on.
The word periodontal literally means 'around the tooth'. Periodontal
disease is most commonly a chronic bacterial infection that affects the
gums and bone supporting the teeth. If left untreated it can lead to
loss of teeth.
Worrying symptoms and signs of periodontal disease warranting urgent referral to an appropriate specialist.
- Rapid progression of symptoms - see 'Aggressive periodontitis', below.
- Unexplained tooth mobility for more than three weeks.
- Unexplained swelling or ulceration of the oral mucosa, lasting for more than 3 weeks - malignancy needs to be ruled out.
- Other suspicions of malignancy: unexplained painful, swollen and bleeding, red or red and white patches on the oral mucosa and unexplained tooth mobility lasting more than 3 weeks.
- Risk factors for malignancy include increasing age (>45 years old), heavy drinking or smoking as well as other use of tobacco (eg chewing).
If a lesion in the oral cavity cannot be diagnosed definitively as benign, follow up for six weeks and, if resolution does not occur, refer urgently to a specialist.
Non-urgent referral to a dentist should be considered for:
- People who cannot use a toothbrush or dental floss.
- Gingivitis not responding to the usual oral hygiene measures.
- Periodontitis.
- Unexplained red and white patches (including suspected lichen planus) or the oral mucosa where there is no swelling, bleeding or pain.
Gingivitis refers to inflammation of the gum of any cause. However, it is most often associated with plaque.
What is plaque? This is the
soft, sticky bacterial deposit that readily forms on exposed surfaces of
teeth. It is easily removed by brushing and flossing. It calcifies over
time, forming tartar (or a calculus) which can only be removed by a
dentist or dental hygienist with special instruments. Plaque results in a
local inflammatory reaction, gingivitis.
Gingivitis is the mildest form of a spectrum disease and it can progress to periodontal disease.
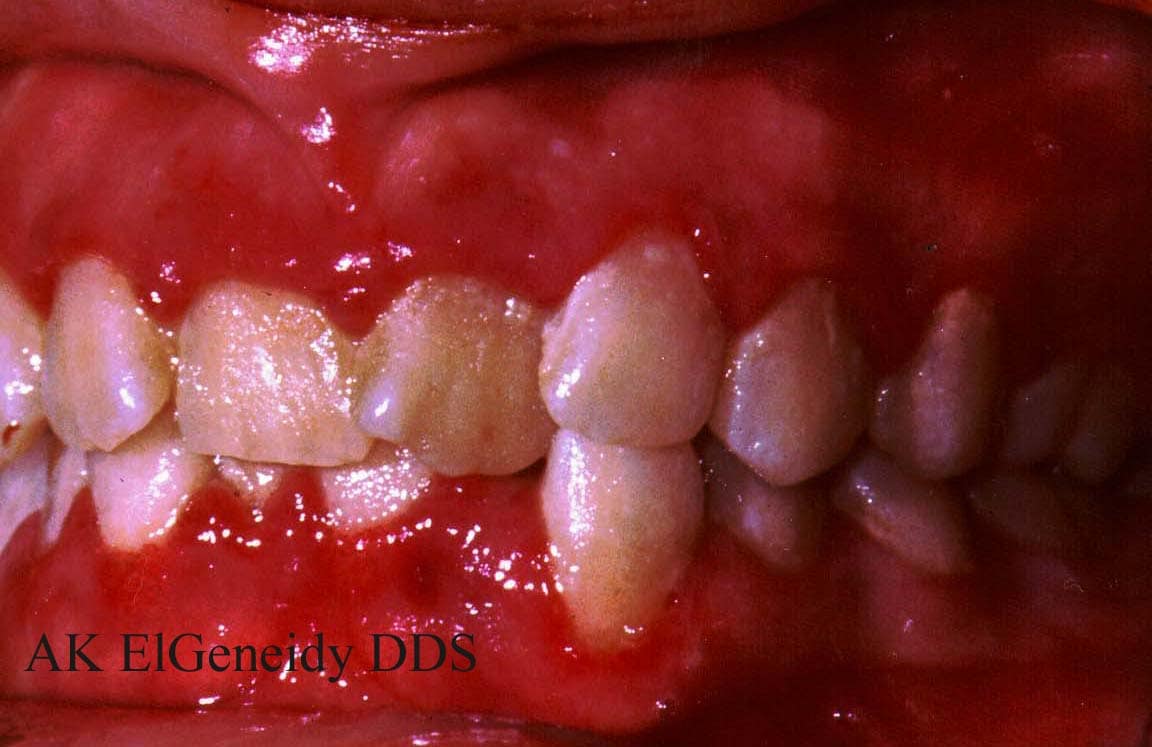
- Presentation - in plaque-associated gingivitis, the
gums become red, swell and bleed easily. There is usually little or no
discomfort. The most important risk factors for this disease are:
- Ineffective oral hygiene
- Cigarette smoking
- Diabetes mellitus
- Other causes of bleeding gums:
- Platelet disorders
- Vitamin C deficiency
- Vascular conditions
- Leukaemia
- HIV infection
- Management - this condition should be managed by a dentist. However, in the interim, advise good oral hygiene (see 'Oral healthcare', below) and use of antiseptic mouthwashes (eg chlorhexidine or hexetidine). This is also an opportunity to address the issue of smoking cessation as this also contributes to periodontal disease.
This is a condition caused by primary infection with the herpes simplex virus, often by contact with someone who has cold sores.
It predominantly (but not exclusively) affects toddlers and young
children and is characterised by an acute onset of fever, malaise, pain
and ulceration of both gingiva and oral mucosa. It may be managed with aciclovir (first episode and child presenting within 3 days of onset on symptoms)[11] or conservatively with simple analgesia and (not aspirin). The episode should fully resolve over about 14 days.
Herpetic gingivostomatitis is common in patients being treated for cancer and a Cochrane review found that aciclovir is effective both for the treatment and prevention of this condition.[12]
Herpetic gingivostomatitis is common in patients being treated for cancer and a Cochrane review found that aciclovir is effective both for the treatment and prevention of this condition.[12]

Also known as Vincent's gingivitis
or trench mouth, this is a progressive, painful, acute bacterial
infection of the gums. The bacteria involved tend to be those already
present in the mouth and it is predominantly associated with anaerobic
flora. Although it is not thought to be infectious, it may occur in
epidemic form, especially in institutions (eg prisons).
- Presentation - sudden onset, acutely painful, bleeding gums, excess salivation and ulceration, swelling and sloughing off of dead tissue. There may be difficulty in swallowing or talking and some report a metallic taste in the mouth. Occasionally, it is accompanied by severe halitosis. Risk factors include immunocompromise, malnutrition, smoking, stress and ineffective oral hygiene.
- Management - these patient should be referred to dentists urgently for immediate treatment and management. Whilst they wait to see the dentist, patients should be prescribed metronidazole or amoxicillin for 3 days, paracetamol or ibuprofen for pain relief and chlorhexidine (0.12% or 0.2%) mouthwash or hydrogen peroxide 6% mouthwash. They should carry on brushing their teeth if possible, using a soft toothbrush.
- Prognosis - if left untreated, it can spread to involve all the gingiva and spread into the bone, forming intraosseous craters (necrotising ulcerative periodontitis). If inadequately treated, it may lead to recurrent ulcerative gingivitis for many years with halitosis, gingival bleeding and recession of the gums. Inadequate treatment can also rarely lead to noma (rapidly spreading gangrene of the lips and cheeks) - more likely in malnourished or immunocompromised individuals.

Untreated gingivitis can advance to periodontitis which is an
inflammation of the periodontal ligament (which attaches the tooth to
the bone) and bone. Toxins produced by the bacteria in plaque irritate
the gums and stimulate a chronic inflammatory response in which the
tissues and bone that support the teeth are broken down and destroyed.
There have been suggestions that periodontal disease might be a risk
factor for cardiovascular disease and pulmonary infection and that its
presence in pregnant women may cause them to have low birthweight or
premature babies.[13][14] However, the evidence is conflicting and further studies are awaited.[15][16] One Indian study has found an association between periodontal disease in pregnancy and the development of pre-eclampsia.[17] A Cochrane review has found some evidence that treating periodontal disease may improve glycaemic control in diabetic patients.[18]
- Presentation - this condition is frequently asymptomatic but, occasionally, the patient may complain of one or more of:
- Pain (which may or may not be caused by an associated periodontal abscess).
- Halitosis or a foul taste in the mouth.
- Recession and associated root sensitivity.
- Drifting/loosening of teeth causing difficulty in eating.
- Management - this is the same as for gingivitis. Ultimately, patients should be seen by a dentist.
- Prognosis - untreated, periodontal disease can lead to permanent damage to the periodontal ligament and alveolar bone. There may be recurrent gum abscesses or detachment of the gum from the tooth with the formation of periodontal pockets. Progressive deepening of periodontal pockets and recession of the gums can lead to drifting and loosening of the teeth, with loss of multiple teeth.
A severe form of periodontists (formerly known as early-onset periodontists) occurs in patients (usually under the age of 35) who are
otherwise clinically healthy. It tends to be associated with Actinobacillus actinomycetemcomitans.
There is rapid loss of dental attachments with loss and destruction of
bone. Familial aggregation may suggest a genetic predisposition or a
poor family tradition of attention to dental hygiene.
Periodontal surgery
 In the early stages of periodontal disease, attention to dental hygiene will suffice. Eating less refined carbohydrate and stopping smoking will also help. Scaling and root planing will also help but surgery may be necessary.
In the early stages of periodontal disease, attention to dental hygiene will suffice. Eating less refined carbohydrate and stopping smoking will also help. Scaling and root planing will also help but surgery may be necessary.There are 4 types of periodontal surgery:
- Pocket reduction surgery - folds back the gum tissue and removes the bacteria before securing the tissue into place. In some cases, irregular surfaces of the damaged bone are smoothed to limit areas where bacteria are sequestered. This allows the gum tissue to reattach to healthy bone.
- Regenerative procedures - these fold back the gum tissue and remove the bacteria. Membranes, bone grafts or tissue-stimulating proteins can be used to encourage the ability to regenerate bone and tissue.
- Crown lengthening - is a procedure to remove excess gum and bone tissue to reshape and expose more of the natural tooth. This can be done to one tooth, to even the gum line, or to several teeth to expose a natural, broad smile. It is a restorative or cosmetic dental procedure. If the tooth is decayed or broken below the gum line, or has insufficient tooth structure for a restoration, it can be extracted and a bridge can be used.
- Soft tissue grafts - stop further dental problems and gum recession and improve the aesthetics of the gum line. Soft tissue grafts can be used to cover roots or develop gum tissue where absent due to excessive gingival recession. Gum tissue from the palate or another donor source covers the exposed root. This can be done for one tooth or several teeth to even the gum line and reduce sensitivity. A soft tissue graft can reduce further recession and bone loss. In some cases, it can cover exposed roots to protect them from decay. This may reduce tooth sensitivity and improve the aesthetics of the smile.
Prevention of gingivitis and periodontal disease requires good oral hygiene (see 'Oral healthcare', below), possible use of antimicrobial mouthwashes and the regular review of a dentist.[19] This is particularly true in diabetics who are more likely to develop infections of the gum and periodontal disease. Other risk factors include puberty and pregnancy as well as bruxism (clenching and grinding of teeth) which can put stress on the structures around the teeth and loosen them. Smoking is also a significant factor in the development and progression of periodontal disease; this is another opportunity to think about stopping smoking.
- Gastrointestinal disease - the mouth is the first part of the alimentary canal and so, in theory at least, history and examination of the gastrointestinal tract should start with the mouth. Think of this when considering Crohn's disease for example.
- Non-gastrointestinal systemic disease - conversely, when looking at lesions in the mouth, bear in mind that there could be a systemic explanation, eg mouth ulcers caused by leukaemia, pemphigus or systemic lupus erythematosus.
- Secondary problems affecting the mouth - the problem you are looking at in the mouth may actually be a secondary problem such as due to insufficient saliva (which is both lubricating and antibacterial, being a good source of immunoglobulin A (IgA)). Disease of both teeth and gums is more common if saliva flow is impaired. This may occur in Sjögren's syndrome, where irradiation to treat cancer may have damaged the glands, in dehydration or when anticholinergic drugs are used.
- Congenital problems - it could be that the problem occurred before you met the patient: all women are screened for syphilis at booking for pregnancy and so congenital syphilis is now very rare in Western societies. One feature is wide-spread peg-shaped teeth called Hutchinson's teeth.
- Childhood problems - developing teeth are also affected by the use of tetracycline which discolours teeth. Profound neonatal jaundice may also stain teeth. Poor intake of calcium in the very early years of life can lead to poor calcification of permanent dentition. Gastrointestinal malabsorption may be to blame but, if a child has cow's milk intolerance and animal milk is replaced by soya milk, this will contain insufficient calcium.
- Iatrogenic problems - finally, drugs may affect both adults and children; for example, phenytoin which can lead to hyperplasia of the gums.
Therefore, when a patient presents with dental or periodontal
problems, take a full history (including medical and drug history),
consider gastrointestinal causes, systemic causes and iatrogenic causes
and, once you are satisfied that these do not apply and the problem is
related purely to the teeth or gums, refer the patient on to a dental
practitioner.
The most important factors for the prevention of both dental and
periodontal disease are a good diet with a minimum of sugar, and
attention to oral hygiene.[20][21] But what do we mean when advising 'good oral hygiene'? Below is a synopsis of the current advice about basic oral healthcare.
- Brush teeth twice a day.
- Floss teeth three times a week.
- Visit a dental practitioner or dental hygienist regularly.
Intervals between visits vary depending on the condition of the teeth
and any treatment received. However, in the absence of specific
conditions needing particular treatment, the National Institute for
Health and Clinical Excellence (NICE) suggests intervals no shorter than
3 months and no longer than 12 months (in those under 18 years old) or
24 months in those over 18 years old.[22]
Regular checks by dentists include scaling of teeth (if required) and the identification and early treatment of caries if it occurs. However, there is a severe shortage of dentists in many parts of the country. Dental health of the population has improved in the last 30 years but this has stagnated in recent years.[23] Much attention is paid to the dental health of children but in old people who still have some teeth it is a problem that is aggravated by regression of gums, reshaping of the mandible and a tendency for saliva volume to diminish.[24]
Regular checks by dentists include scaling of teeth (if required) and the identification and early treatment of caries if it occurs. However, there is a severe shortage of dentists in many parts of the country. Dental health of the population has improved in the last 30 years but this has stagnated in recent years.[23] Much attention is paid to the dental health of children but in old people who still have some teeth it is a problem that is aggravated by regression of gums, reshaping of the mandible and a tendency for saliva volume to diminish.[24]
Older people, institutionalised patients, patients with mental health
problems and individuals with a learning disability may face particular
challenges in managing their oral health. Problems may be experienced
due to:
- Barriers in accessing adequate oral care due to lack of perceived need, inability by the individual to express need and a lack of ability to self-care.
- Fear and anxieties, which are also significant contributors to poor access to oral care providers.
- The knowledge and skills of carers may be inadequate.
- Concurrent illness may take priority and oral healthcare takes a back seat.
Detailed guidance for these specific patient groups are more within
the remit of dental practitioners. However, documents outlining these
recommendations are included in the further reading section - integrated
care pathways are used and there will be an overlap of the services
provided to the individual (and these may include the general
practitioner).
The first link provided in the Internet and further reading section
below can be used to find a local NHS dentist: names, locations and
opening hours are provided. It also provides information regarding
charges and a number of helpful links to related websites.

This logo signifies that the product has been approved by the British
Dental Health Foundation and is a useful guide as to the quality of the
item.
- Relief of toothache:
- Papyrus records detail Egyptian remedies such as stone powder, ocher
(iron ore) and honey. Other civilizations developed plant remedies,
including cloves, pepper, cinnamon, poppy seeds, ginger, copal (resin
from trees), mint and tobacco.
- Papyrus records detail Egyptian remedies such as stone powder, ocher
(iron ore) and honey. Other civilizations developed plant remedies,
including cloves, pepper, cinnamon, poppy seeds, ginger, copal (resin
from trees), mint and tobacco.
- Removal of the tooth and substitution with artificial replacement:
- Extraction was practised by the Egyptians and in ancient Greece. Hippocratic literature devoted many paragraphs to dental care and included a numbering system for teeth.
- In Roman times the Etruscans of central Italy made crowns and bridges, gold bands holding cadaver or calf teeth, or artificial teeth made from ivory or bone, though these soon rotted.
- This skill was largely lost until the 1800s, Elizabeth I using cloth to fill the holes in her mouth to improve her appearance in public.
- A French pharmacist Duchateau, with dentist Dubois de Chemant, designed the first hard-baked, rot-proof porcelain dentures in 1774 and the Englishman Claudius Ash invented an improved porcelain tooth around 1837.
- With Charles Goodyear's discovery of vulcanised rubber in 1839 (a
cheap, easily worked, mouldable base for false teeth) and Horace Wells'
discovery of nitrous oxide for painless teeth extraction in 1844,
dentures became popular.
- Removal of decay and restoration:
- The oldest filling is >2,000 years old, being a piece of bronze wire inserted into the root canal of a Nabetan warrior in Egypt, believed to prevent 'tooth worms' being thought as the cause of decay well into the Middle Ages.
- In the Middle Ages resins, waxes and gums were used as fillings, with lead and gold introduced shortly after.
- The Frenchman Pierre Fauchard is considered the father of modern dentistry, developing an improved drill in 1728. He favoured tin foil or lead cylinders for fillings.
- US dentist Robert Arthur developed the cohesive gold foil method in 1855.
- Amalgam (silver, or its alloys, combined with mercury) was developed
by the Frenchman Auguste Taveau in 1816, with fears of leaky fillings
and the effect of mercury on health surfacing quickly. These were not
assuaged until the work of Chicago dentist G V Black in 1895 who
standardised both cavity preparation and amalgam manufacture.
- Prevention:
- In ancient India and China medical writings recommended a toothbrush made from a frayed twig, and both tongue scrapers and toothpicks were in use.
- An American dentist trained his office assistant as a dental hygienist in 1906 and set up the first hygienist course in 1913 in Bridgeport, Connecticut. This led to the first dental public health programme.
The author is grateful to Dr D J Ward for his additions in the historical section.
Further reading & references
- Clinical Guidelines & Integrated Care Pathways for the Oral Health Care of People with Learning Disabilities; Clinical Guidelines & Integrated Care Pathways for the Oral Health Care of People with Learning Disabilities, British Society for Disability and Oral Health (2001)
- Guidelines for oral health care for long-stay patients and residents, British Society for Disability and Oral Health (2000)
- Guidelines for oral health care for people with a physical disability, British Society for Disability and Oral Health (2000)
- Preventing Dental Caries in Children at High Caries Risk. Targeted prevention of dental caries in the permanent teeth of 6-16 year olds presenting for dental care, Scottish Intercollegiate Guidelines Network - SIGN (2000)
- Tooth decay - HealOzone, NICE (2005)
- Principles on Intervention for People Unable to Comply with Routine Dental Care, British Society for Disability and Oral Health (2004)
- The Development of Standards for Domiciliary Dental Care Services: Guidelines and recommendations, British Society for Disability and Oral Health (2000)
- Find and choose services, NHS Choices
- Polhaus S; (American) Private Dentistry website with excellent resources for lay-people and professionals. Site has good images
- Marinho VCC, Higgins JPT, Logan S, Sheiham A.; Topical fluoride (toothpastes, mouthrinses, gels or varnishes) for preventing dental caries in children and adolescents. Cochrane Database of Systematic Reviews 2003, Issue 4. Art. No.: CD002782. DOI: 10.1002/14651858.CD002782.
- Prevention and management of dental decay in the pre-school child, Scottish Intercollegiate Guidelines Network - SIGN (2005)
- FAQs: fluoridation, British Dental Health Foundation
- British Fluoridation Society; Action group promoting the benefits of fluoride
- All Party Parliamentary Group Against Fluoridation; Action group against fluoridation
- NHS Evidence; 2010 Oral Health Annual Evidence Update - Dental Caries
- Dental abscess, Clinical Knowledge Summaries (January 2008)
- Wisdom teeth removal; NICE Technology appraisal, 2003; Summary of advice
- Blinkhorn AS, Mackie IC; My child's just knocked out a front tooth. BMJ. 1996 Mar 2;312(7030):526.
- Gingivitis and periodontitis - plaque-associated, Clinical Knowledge Summaries (2007)
- Amir J, Harel L, Smetana Z, et al; Treatment of herpes simplex gingivostomatitis with aciclovir in children: a randomised double blind placebo controlled study. BMJ. 1997 Jun 21;314(7097):1800-3. [abstract]
- Glenny AM, Fernandez Mauleffinch LM, Pavitt S, et al; Interventions for the prevention and treatment of herpes simplex virus in Cochrane Database Syst Rev. 2009 Jan 21;(1):CD006706. [abstract]
- Jeffcoat MK, Geurs NC, Reddy MS, et al; Periodontal infection and preterm birth: results of a prospective study. J Am Dent Assoc. 2001 Jul;132(7):875-80. [abstract]
- Lopez NJ, Smith PC, Gutierrez J; Periodontal therapy may reduce the risk of preterm low birth weight in women with periodontal disease: a randomized controlled trial. J Periodontol. 2002 Aug;73(8):911-24. [abstract]
- Moore S, Ide M, Coward PY, et al; A prospective study to investigate the relationship between periodontal disease and adverse pregnancy outcome. Br Dent J. 2004 Sep 11;197(5):251-8; discussion 247. [abstract]
- Oliveira AM, de Oliveira PA, Cota LO, et al; Periodontal therapy and risk for adverse pregnancy outcomes. Clin Oral Investig. 2010 May 22. [abstract]
- Shetty M, Shetty PK, Ramesh A, et al; Periodontal disease in pregnancy is a risk factor for preeclampsia. Acta Obstet Gynecol Scand. 2010 May;89(5):718-21. [abstract]
- Simpson TC, Needleman I, Wild SH, et al; Treatment of periodontal disease for glycaemic control in people with diabetes. Cochrane Database Syst Rev. 2010 May 12;5:CD004714. [abstract]
- Coventry J, Griffiths G, Scully C, et al; ABC of oral health: periodontal disease. BMJ. 2000 Jul 1;321(7252):36-9.
- Harris R, Nicoll AD, Adair PM, et al; Risk factors for dental caries in young children: a systematic review of the literature. Community Dent Health. 2004 Mar;21(1 Suppl):71-85. [abstract]
- Sanders TA; Diet and general health: dietary counselling. Caries Res. 2004;38 Suppl 1:3-8. [abstract]
- Dental recall - Recall interval between routine dental examinations, NICE (2004)
- Pitts NB, Boyles J, Nugent ZJ, et al; The dental caries experience of 14-year-old children in England and Wales. Surveys co-ordinated by the British Association for the Study of Community Dentistry in 2002/2003. Community Dent Health. 2004 Mar;21(1):45-57. [abstract]
- Atkinson JC, Grisius M, Massey W; Salivary hypofunction and xerostomia: diagnosis and treatment. Dent Clin North Am. 2005 Apr;49(2):309-26. [abstract]
| Original Author: Dr Olivia Scott |
| Current Version: Dr Laurence Knott |
Disclaimer: This article is for information only and should not be used for the diagnosis or treatment of medical conditions. EMIS has used all reasonable care in compiling the information but make no warranty as to its accuracy. Consult a doctor or other health care professional for diagnosis and treatment of medical conditions. For details see our conditions.
[ Collected from this website ]











