Duh. You’ve only been
hearing that since you were too small to really understand what it
meant, but the importance of daily brushing and flossing can not be
overstressed. Even as adults who should know better, we often skip
flossing because it’s too painful, time-consuming, or boring.
Why
are brushing and flossing so critical to your health? Every day,
bacteria grow in our mouths. During the day, saliva washes away much of
it, but at night it happily multiplies in the warm, moist environment.
At night, you produce less saliva, so the bacteria are less likely to be
washed away. The more bacteria you allow to settle on to your teeth and
gums, the more likely you are to develop cavities (which is why those bacteria are so often called “cavity bugs” by your friendly dentist), halitosis (bad breath), and gum disease.
Brushing
twice a day for two minutes at a time – in the morning and before bed –
is a way of removing the bacteria and keeping your mouth cleaner. Use a
soft manual toothbrush or electric brush and gently scrub your teeth
and gums in a circular motion, being careful to get all the way back to
your back teeth
Flossing is just as necessary as brushing. Your
toothbrush can remove bacteria and plaque from the outside surfaces of
your teeth, but most cavities start as food decays between your teeth,
and abscesses, other infections, and gum disease can be triggered by
these unattended cavities. Flossing daily in the evening scrapes out
bits of food that would otherwise feed the bacteria in your mouth. If
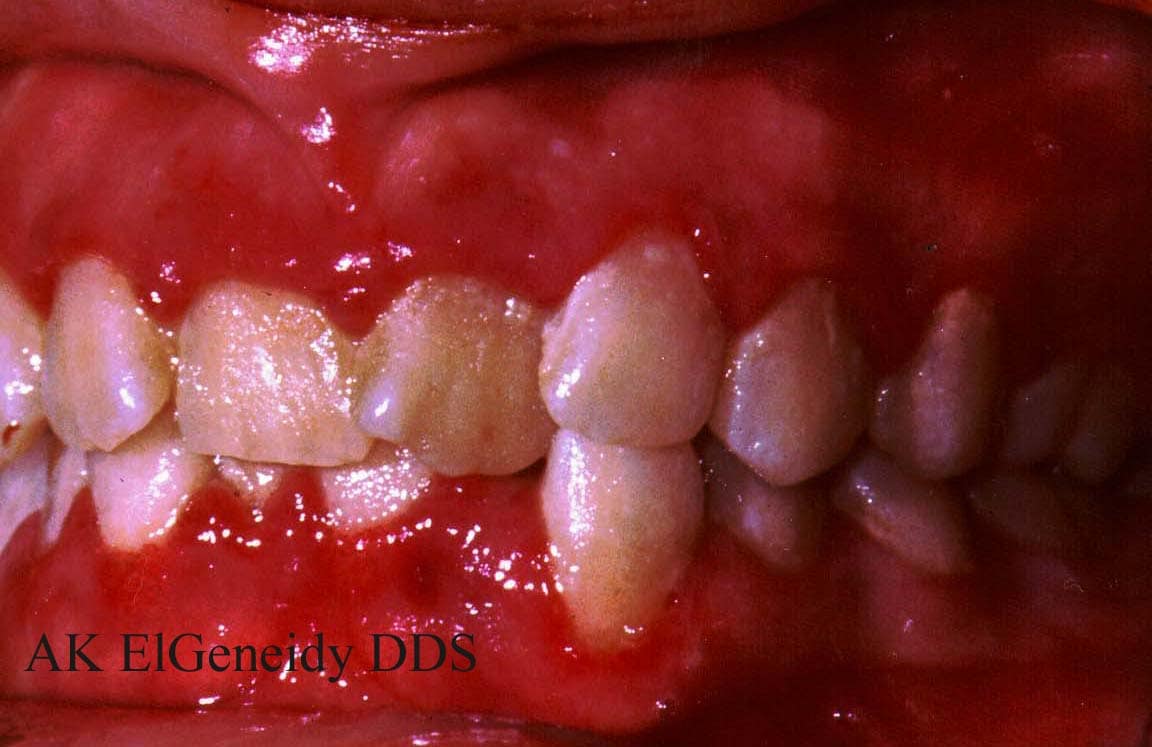
you haven’t flossed in a while, your gums might bleed a little, but
after a couple of days of gentle flossing, your gums will toughen up.
There
are a variety of flosses available, as well, and you can pick exactly
the type you like best and that feels good in your mouth. Not only can
you choose from the old-fashioned waxed and unwaxed flosses, you can
also select a dental tape, which is like a flat ribbon – perfect for
sliding between close-set teeth – or single use flossing gadgets where
the floss is already tightly attached to a Y-shaped handle, allowing you
to easily maneuver the floss one-handed through your mouth. Floss also
comes covered in mint to keep your breath smelling bright and fresh. It
only takes about 30 seconds to efficiently floss your teeth by sliding
the floss side to side and up and down along each of the inner edges
between your teeth. Again, don’t miss the back edges of your wisdom
teeth. Wisdom teeth are often overlooked and under-flossed, and the
neglect makes them prime candidates for decay and infection.
Fruits
and vegetables in their whole form – with skin on, if appropriate –
provide vitamins, minerals, and other nutrients vital to your body’s
overall health. Crunching on apples and carrots also keeps your teeth in
top form, as long as the apples and carrots aren’t also sticking around
between your teeth at night. Eating deep, leafy greens such as kale,
chard, and spinach also provide calcium, which is essential for bone
mass. Bone mass and exercise help your teeth in a way we’ll talk about
in just a moment.
You know
you should stay away from sweets, as sugar is bacteria’s favorite fuel
and it doesn’t do your body any good whatsoever. Since it’s nearly
impossible to abstain completely, extra brushing after eating sugary
foods can help you get fewer cavities.
It
may be surprising that exercise can benefit your teeth and gums, but
research has shown that exercise increases bone mass. When you begin to
suffer from osteoporosis, or a gradual loss of bone density that causes
bones to become porous and more fragile, your body will steal calcium,
phosphorous, and other minerals from your mouth and jaw in order to
maintain the support structure of your skeleton. You might notice that
your gums are receding and bleeding during brushing. Your jaw can also
become severely weakened.
Exercise and a diet that includes lots
of the necessary nutrients – like calcium and phosphorous – that support
proper bone density will also keep your mouth happy. Make sure you also
get a good dose of Vitamin D, which you can either take in through
sunlight or with supplements.
Visiting your dentist every six months for checkups should be a no-brainer, but getting wayward teeth into shape by visiting an orthodontist in Manhattan,
Oceanside, or Duluth – wherever you happen to live – is also important.
Teeth that grow in crookedly can be teeth that become unhealthy. Not
only will the proper methods of straightening or correcting dental
abnormalities help you love your smile, it will be easier to keep your
teeth clean and healthy. Psychologically, if you love your smile, you
are also more likely to be vigilant in keeping it white and bright.
Aside
from crooked teeth, an orthodontist can help you solve other problems,
such as tooth grinding and TMJ, both of which damage your teeth and jaw
over time.
Tooth health doesn’t just affect your mouth. It affects
your entire body. Keeping your teeth and gums happy also means you are
less prone to other illnesses and infections, and keeping your body
happy and healthy means your mouth is less susceptible to disease.

I get a lot of questions about dental hygiene and health, and for good reason.
Dental records of our paleolithic ancestors show a fairly low incidence of caries when compared to modern teeth.
Exceptions exist, but the general trends suggest that
Grok
had better teeth than the average contemporary human. Of course, when
cavities struck back then, they hit hard and got really ugly, because
there were no dentists, drills, or x-rays to fix the problem, but most
never got to that point. Also, the adoption of agriculture is generally
associated with the emergence of poor dental health, so much so that
many researchers use the appearance of
dental caries in a population as strong evidence for the presence of farming.
Maize/corn is particularly bad, as is wheat, but the same relationship
may not hold true for rice agriculture in Asian records.
Okay – let’s take a look at a couple common questions I get about dental health:
Mark, this morning as a dental assistant was making my
head buzz and my gums hurt with some sort of ultrasonic tooth cleaner, I
thought, “what can Grok teach us about tooth care?” Something tells me
Grok did not brush his teeth–did he do anything to take care of himself
in that way? And if he survived just fine, what does that tell us about
“conventional wisdom” that says we should adopt a routine, and buy a
medicine cabinet full of stuff to take care of our teeth? I certainly
don’t mean to convey that tooth care is bad–but rather am just thinking
about what we can learn from the past to harmonize the present.
Thanks for reading this, and thank you for your dedication to better health!
Hey Mark! I’ve recently taken an interest in making my
oral regimen more Primal. I’ve read up on a lot of the more natural
toothpastes and toothpaste alternatives but I’m undecided. What have you
and your wife found to be the safest and most effective way to keep
your cavities at bay?? Thanks!
Before resorting to anything reactive, whether it be brushing with
homemade toothpaste, dousing your oral cavity with anti-bacterial
mouthwash, bypassing the teeth altogether with an IV nutrient feed, or
using a dental dam to chew, those seeking excellent dental health should
establish a strong dietary foundation of the minerals, micronutrients,
and other cofactors that play major roles in the maintenance of teeth.
You’ve probably heard about how this holy trinity of micronutrients
works together to promote proper bone and tooth mineralization, which
means putting calcium and other minerals where they belong (bones,
teeth) instead of where they don’t (arteries, dental calculus/plaque).
Both
Stephan Guyenet and
Chris Masterjohn
have written extensively about the synergistic interplay between the
three nutritional factors, so I’ll keep this brief. Get adequate midday
sun or take
vitamin D supplements; eat
grass-fed butter, hard cheeses, and
organs (especially goose liver, apparently), or supplement with vitamin
K2; get plenty of vitamin A from liver, egg yolks, and other animal products.
I probably don’t have to tell
you to
avoid grains, but for any newcomers who might be reading: ditch the grains,
beans, and other legumes
that contain high levels of phytic acid, which is known to bind to and
prevent absorption of minerals critical for dental health.
Nuts
also contain phytic acid, but we tend not to eat as many nuts as grains
or legumes due to the caloric load. It’s a lot easier to eat two cups
of whole wheat than it is to eat two cups of almonds. If you do eat nuts
on a regular basis, consider
soaking and/or sprouting them to reduce phytic acid content.
It’s not enough to consume the holy mineralization trio and avoid
excessive amounts of mineral-binding phytic acid; you also need the raw
building blocks. That means getting plenty of minerals in your diet.
Leafy greens,
grass-fed meat, organs, nuts,
roots, and tubers are all good Primal sources of calcium, phosphorous, magnesium, and other vital micronutrients – vital for general
and dental health – so eat plenty of them.
There are numerous examples of traditional cultures using chewing
sticks from trees with medicinal or antimicrobial properties, like the
neem in India, the
miswak/arak in Africa, the Mid East, and Asia, or the tea tree, which I mentioned in a
previous post. Here’s an
example
of a Masai “toothbrush” – it’s a whittled-down branch from a (perhaps
medicinal) tree with the end frayed and the fibers splayed out to permit
interdental entry. If you don’t have access to a miswak, neem, or tea
tree, you can find
chew sticks online quite easily. Toothpicks or floss will also work pretty well as a physical deterrent, albeit without any medicinal qualities.
There isn’t a ton of head-to-head research on the subject, but
one study
from 2003 found that miswak chewing sticks removed more plaque and
resulted in better gingival health than toothbrushes. The caveat is that
chew stick users had to be instructed in the proper use of the
implements, whereas toothbrushes are fairly straightforward (not to
mention most of us have grown up using them, so we’re well-versed in
toothbrushing). It’s notable that chew sticks do not require toothpaste,
and they appear to be just as, if not more, effective than
toothbrushes. Longer history of use, too. You just have to know how to
use it. Miswak appears to be the most studied, so you’ll probably want
to use that variety.
If you’re gonna use a toothbrush, do you need the paste? If so, is
Crest/Colgate/insert-mainstream-paste-here good, or should you go with
an herbal/alternative/insert-paste-available-at-Whole-Foods-here
instead?
Toothpaste use
increases abrasion
during brushing, while water alone produces less abrasive force.
Interestingly, the same study revealed that softer toothbrushes actually
cause as much abrasion (and sometimes more) than stiffer toothbrushes.
While increased abrasive forces seem like they’d reduce more plaque,
that doesn’t seem to be the case. A recent study found that the brushing
is the important part, not the paste. In fact, brushing without paste
was
more effective at removing plaque than brushing with paste.
An herbal toothpaste made from herbs and plants traditionally used to treat oral disease in India was
superior to a placebo toothpaste in the treatment of gingival bleeding and oral hygiene.
Another study
compared herbal toothpastes to conventional fluoride-containing
toothpastes in the treatment of established gingivitis and found that
both were equally effective.
In
another study, a baking soda toothpaste beat an antimicrobial non-baking soda toothpaste in plaque removal and tooth maintenance.
Most studies,
in fact, show that baking soda is more effective at plaque removal than
toothpastes without baking soda. It’s pretty common among older folks
to just use straight baking soda to brush, and this seems to be an
effective tactic.
If you’ve got all the nutritional and environmental cofactors under
control, I don’t think obsessive dental hygiene beyond daily brushing
(remember, even if the bristly toothbrush is a recent invention,
cleaning our teeth with sticks or picking at them with fingernails is
tradition), some toothpicking/flossing, regular dental visits, and/or
maybe some chew sticking is necessary. It doesn’t even seem like
toothpaste is necessary for good oral health. That said, I do use it –
perhaps because I’ve just become conditioned to, or maybe because I need
the artificially fresh feeling it provides – but I also don’t feel the
pressing need to brush on schedule. I just don’t develop a ton of plaque
if I go a bit longer than normal without brushing, nor do I get bad
breath. And as anyone who’s been married for more than ten years will
tell you, the wife will definitely let you know if things go awry in
that area. If you want a cheap toothpaste that isn’t overly sweet,
baking soda should do the trick.